J. Biosci. Public Health. 2025; 1(1)
Dengue fever presents with a broad spectrum of symptoms, ranging from mild to life-threatening complications. Understanding the clinical symptoms based on demographic and biochemical predictors of severity is vital for early intervention. A cross-sectional study was conducted among 375 dengue patients. Clinical symptoms, demographic profiles, platelet counts, and infection history were analyzed. Then the level of severity has been categorized as Dengue Fever (DF), Dengue Fever with Warning Signs (DFWS), and Severe Dengue (SD), emphasizing warning signs like abdominal pain, nausea/vomiting, and hemorrhage as indicators of severity. Results show males were more affected, while females exhibited more severe symptoms, including hypotension, and hemorrhage. Pediatric patients showed higher prevalence of warning signs, such as abdominal pain and poor appetite, suggesting increased severity risk. Among occupations, homemakers had the highest incidence of warning signs, potentially due to delayed healthcare access and domestic mosquito exposure. Severe thrombocytopenia (<20k/μL) was associated with low blood pressure and hemorrhage. Secondary infections showed a strong association with severe manifestations, supporting the role of antibody-dependent enhancement. Female gender, younger age, homemaker occupation, low platelet counts, and secondary infections were strongly linked with severe dengue. These findings highlight the need for early detection of the severity level of dengue infections and management strategies to prevent disease progression in high-risk groups.
Dengue fever, a mosquito-borne viral disease caused by the dengue virus (DENV), remains a significant public health challenge in tropical and subtropical regions. Prevalent dengue presents a spectrum of clinical manifestations, ranging from mild febrile illness to severe conditions such as Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS) [1]. According to the WHO 2009 guidelines, which classify dengue into Dengue Fever (DF), Dengue Fever with Warning Signs (DFWS), and Severe Dengue (SD), emphasizing warning signs like abdominal pain, nausea/vomiting, and hemorrhage as indicators of severity [2]. As a major global health concern, dengue affects over 50% of the world’s population living in endemic regions, particularly impacting Southeast Asia, sub-Saharan Africa, and Latin America [3]. A brief summary of the situation over 7.6 million dengue cases, including 3.4 million confirmed cases, over 16,000 severe cases, and over 3,000 deaths, were reported to the WHO as of April 2024 [4]. Bangladesh, located in the dengue-endemic Southeast Asian region, faces significant public health challenges due to recurrent outbreaks.
In Bangladesh, dengue has been a growing public health concern since a major outbreak in 2000. In the past two years alone, the country reported 321,017 cases with 1,122 deaths in 2023 and 101,211 cases with 575 deaths in 2024. According to the report, Dhaka, the capital, consistently reports the highest number of cases [5, 6]. Phylogenetic studies indicate that the 2000 epidemic in Bangladesh was likely driven by the introduction of a virulent DENV-3 strain (Asian genotype II), closely related to strains circulating in Thailand and Myanmar [7]. Seasonal patterns show that dengue cases peak during the monsoon (May–August) and post-monsoon (September–December) seasons in Bangladesh [8]. Since 2018, dengue cases in Bangladesh have shown an upward trend, with 2023 marking a record-breaking outbreak—over 300,000 reported cases. Only in September 2023 were a maximum of 79,598 dengue cases reported [9].
Dengue transmission is significantly influenced by temperature and viral strain. In humans, the incubation period, the time between infection and symptom onset, typically ranges from 4 to 7 days but can vary between 3 and 10 days [3]. Approximately 80% of infections are asymptomatic or mild, 5% result in severe illness, and less than 1% are fatal despite treatment [10]. Therefore, the clinical manifestations of dengue vary widely. Mild cases, often termed dengue fever (DF), are characterized by symptoms such as fever, arthralgia (joint pain or stiffness), myalgia (muscle pain or soreness), retro-orbital pain, and skin rash [3, 11]. Severe cases may involve hemorrhagic manifestations and complications like thrombocytopenia, abnormal liver function, nausea-vomiting, respiratory symptoms, and abdominal pain etc [12]. Secondary infections or infections with particularly virulent strains are associated with increased severity, potentially leading to life-threatening complications such as shock or organ dysfunction, pulmonary edema, or significant bleeding [13]. Several studies have identified demographic, immunological, and environmental factors as key determinants of dengue severity, including age, prior DENV exposure, viral serotype, and host genetic factors [14]. Therefore, understanding the factors influencing these clinical manifestations is critical for predicting disease severity and improving patient outcomes.
This patient-based study aims to investigate the influence of sociodemographic and health-related factors on the prevalence of clinical symptoms, distribution patterns, and severity level of dengue patients in Dhaka, Bangladesh. The findings of this study are anticipated to provide valuable insights for policymakers in formulating effective dengue prevention strategies. Furthermore, these findings may raise public awareness of the factors affecting dengue fever severity, especially in Bangladesh.
Study Design
This cross-sectional observational study was conducted from April 2022 to March 2023 in Dhaka, Bangladesh. Data were collected from three hospitals and healthcare institutions. Formal permission was obtained from all participating institutions prior to data collection. In this study, a total of 375 dengue patients were participated as our study population. All of them are living in the Dhaka metropolitan area. All the participants were confirmedly diagnosed with dengue infection according to the clinical report and decision of the physician based on their serological evidence (positive dengue NS1 antigen or IgM antibody). Patients’ demographic information, clinical symptoms, and physical complications-related data were recorded by direct interview following a well-structured questionnaire.
Inclusion criteria were (i) only laboratory-confirmed dengue infection patients and (ii) willingness to participate in this study. Exclusion criteria included (i) pregnant women, (ii) patients who declined participation, and (iii) cases with mixed infections (e.g., co-infection with chikungunya virus or other pathogens).
Data Collection
After obtaining informed consent, data were collected through patient interviews using a structured questionnaire. The questionnaire captured sociodemographic information, including age, sex, occupation, and residential area. It also recorded others' medical history, like any previous record of dengue infection. Additionally, clinical and biochemical data were gathered, encompassing self-reported symptoms like fever, headache, muscle and joint pain, rash, hemorrhage or bleeding, physical weakness, and gastrointestinal complaints, collected from medical records where it was available and patients’ statements. For children (below 18 years), they took support from their guardian to ensure every piece of data.
Sample Size calculation
The sample size was calculated using the following equation [15]:
Here, n = number of samples
z = critical value of the normal distribution
p = expected prevalence estimate
q = (1-p) = expected non-prevalence
d = precision limit or proportion of sampling error
The critical value (z) is included as 1.96 for a 95% confidence level. The precision limit, or proportion of sampling error (d), is usually considered to be a 5% confidence limit.
Therefore,
≈ 375 participants were estimated.
Statistical Analysis
Data were analyzed using IBM SPSS statistics for Windows, Version 24.0, and Microsoft Excel. Descriptive statistics were calculated for all variables. Associations between categorical variables were assessed using the chi-square test or Fisher’s exact test, as appropriate. Continuous variables were compared using independent samples t-tests or one-way analysis of variance (ANOVA), depending on the number of groups. Assumptions of normality and homogeneity of variances were checked prior to applying t-tests and ANOVA. A p-value of <0.05 was considered statistically significant.
Ethical Consideration
All procedures followed the principles of the Helsinki Declaration. Participants were informed about the study's purpose, procedures, and confidentiality, and provided voluntary consent. Written consent was also obtained from the parents or guardians before data collection using a structured questionnaire.
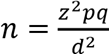
The demographic characteristics of the 375-study population have been depicted in Table 1. Here, the percentage of males was almost double (63%) compared to females (37%). Populations ranging in age from one to over 45 years old were chosen. The maximum number of participants in this study were within the age range of 35 years. More specifically, 26% of children are in the pediatric range below 18 years, whereas 46% are between 18 and 35 years old. In this study, approximately 14% of the participants were over the age of 45. In terms of occupation, approximately 29% were students, 26% worked, and 17% were housewives. About 20% of participants were involved in various professions like rickshaw pullers, day laborers, motor drivers, street vendors, etc.
Table 1. Distribution of sociodemographic characteristics of the study population (N = 375).
After presenting demographic information, the distribution of all recorded clinical manifestations of dengue patients has been summarized in Figure 1. The histogram displays the frequency of clinical symptoms and their prevalence, with fever affecting 100% (375), physical weakness at 93.9% (352), poor appetite at 66.7% (250), joint and muscle pain at 67.5% (253), skin rash at 27.2% (102), nausea and vomiting at 58.9% (221), abdominal pain at 74.9% (281 cases), low blood pressure at 38.2% (143), cough at 23.2% (87), hemorrhage at 24% (90), and diarrhea at 14.7% (55).
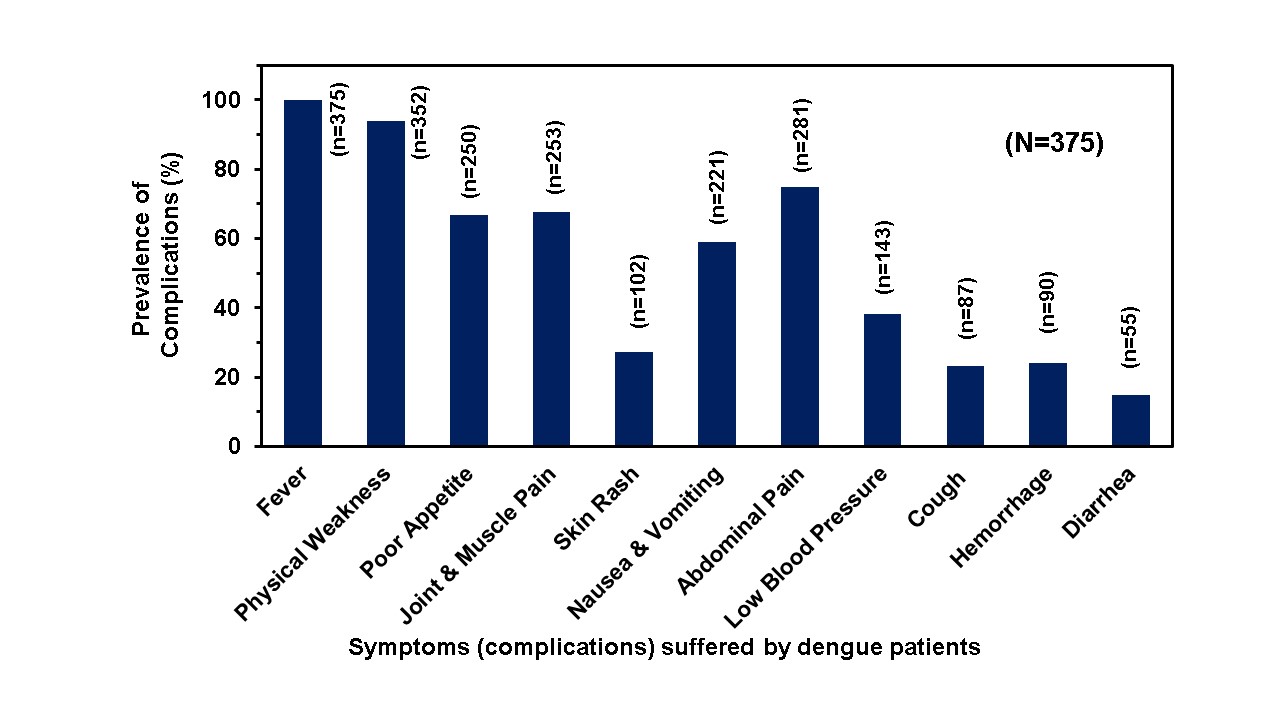
Figure 1. Distribution summary of reported clinical symptoms (complications) suffered by dengue patients (N= 375).
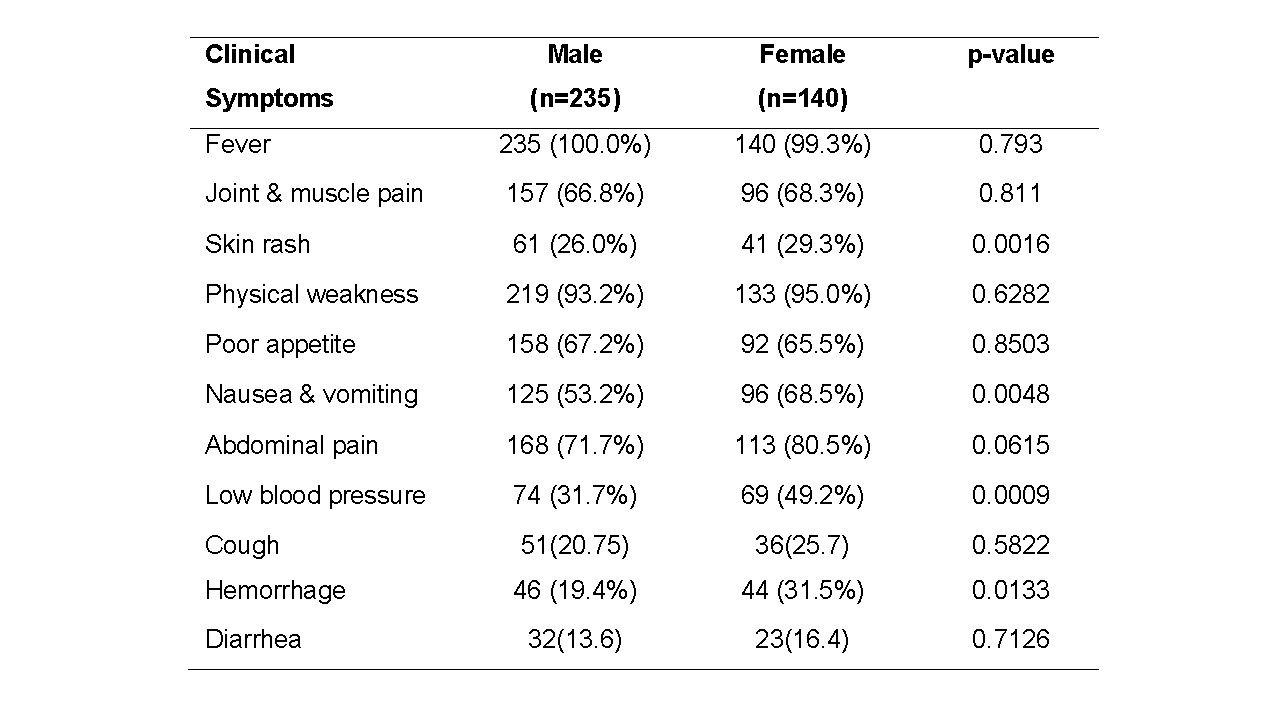
Now, correlation of clinical symptoms with various demographic as well as biochemical factors has been investigated sequentially. As shown in Table 2, gender-stratified variations in clinical symptoms of 374 dengue patients (235 males and 140 females) in Bangladesh. Fever was the most common symptom across both sexes. Although physical weakness, poor appetite, joint and muscle pain, abdominal pain, and diarrhea were highly prevalent in both genders, no significant gender-based differences were observed for these symptoms. However, skin rash (29.3% in females vs. 26.0% in males; p = 0.0016), nausea and vomiting (68.5% in females vs. 53.2% in males; p = 0.0048), low blood pressure (49.2% in females vs. 31.7% in males; p = 0.0009), and hemorrhage (31.5% in females vs. 19.4% in males; p = 0.0133) were significantly more frequent among female patients, indicating potential gender-based disparities in the clinical presentation of dengue in this population.
Table 2. Health problems during dengue based on the gender.
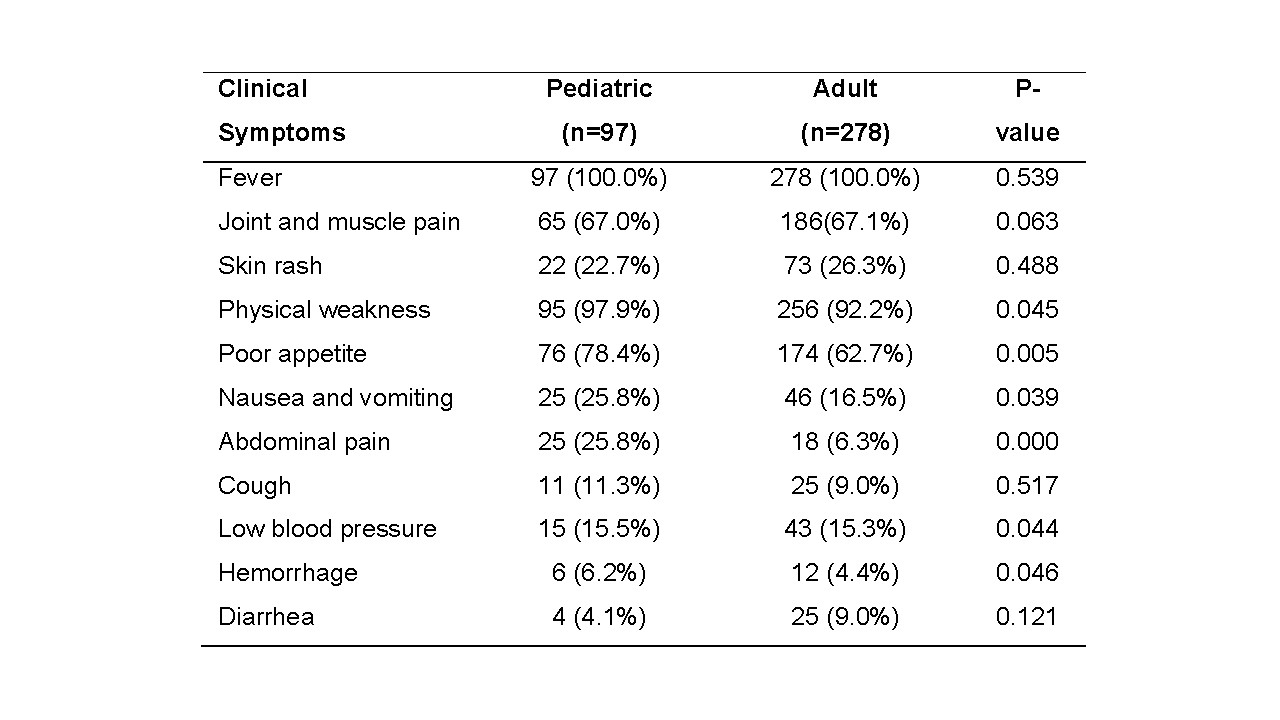
Here, age-dependent clinical symptoms among pediatric and adult dengue patients have been uncovered in Table 3. While rates of fever were nearly universal in both age groups. Otherwise, in the case of pediatric patients, physical weakness (97.9% vs. 92.2%; p = 0.045), poor appetite (78.4% vs. 62.7%; p = 0.005), nausea and vomiting (25.8% vs. 16.5%; p = 0.049), abdominal pain (25.8% vs. 6.3%; p = 0.000), low blood pressure (15.5% vs. 15.3%; p = 0.048), and hemorrhage (6.2% vs. 4.3%; p = 0.046) rates were significantly higher than those of adult patients. In contrast, no significant differences were observed for joint and muscle pain, skin rash, cough, or diarrhea between the age groups. These findings suggest that pediatric patients exhibit a higher prevalence of warning signs, indicating a greater chance of progression to severe dengue compared to adults.
Table 3. Age-Based comparison of clinical symptoms in dengue patients (N=375).
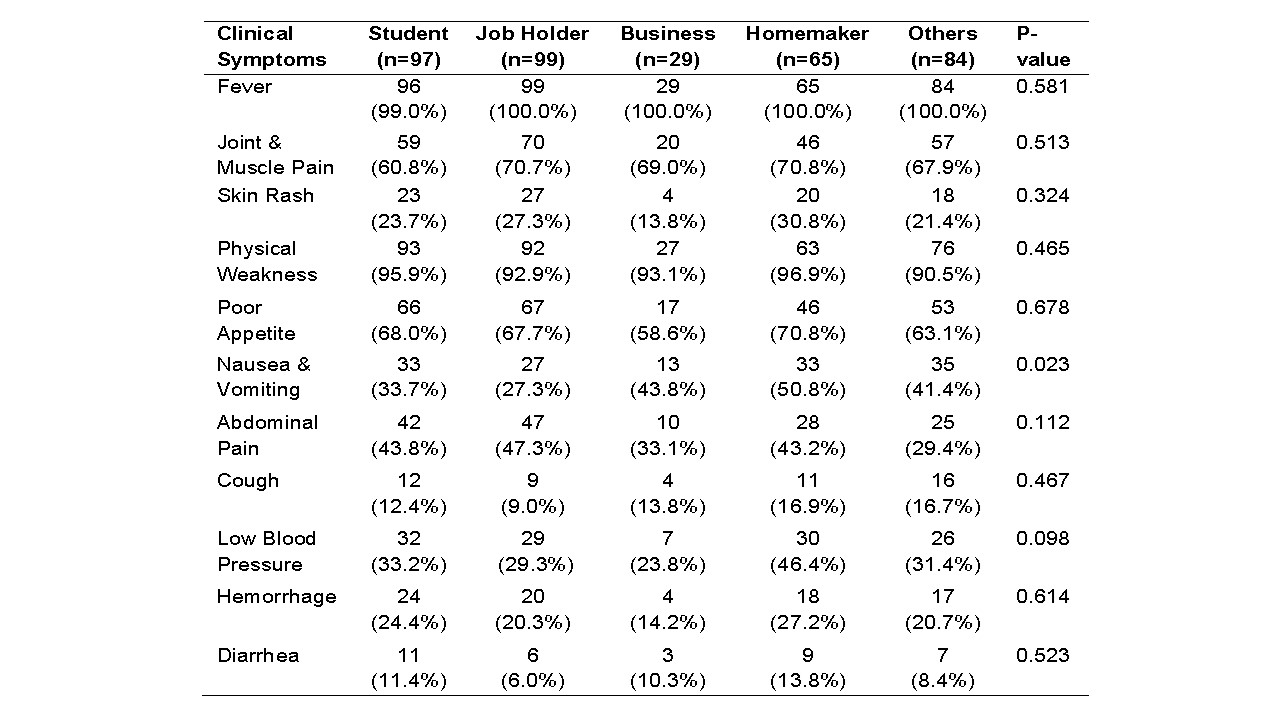
Next, the findings in Table 4 present the comparative prevalence rate of clinical symptoms of dengue by the occupation of patients. Fever and physical weakness were very common. There was no noticeable statistical correlation between the professions, and complications of nausea differed greatly (p=0.023), with job holders experiencing the lowest rate (27.3%) and homemakers reporting the highest rate (50.8%). In contrast, the frequency of joint and muscular pain (60.8%–70.8%, p=0.513), poor appetite (58.6%–70.8%, p=0.678), hemorrhage (14.2%–27.2%, p=0.614), skin rash (13.8%–30.8%, p=0.324), cough (9.0%–16.9%, p=0.467), and diarrhea (6.0%–13.8%, p=0.523) were the only symptoms that did not differ significantly. Low blood pressure was most prevalent among homemakers (46.4%) and least prevalent among business owners (23.8%, p=0.098), whereas abdominal pain varied from 29.4% (others) to 47.3% (job holders, p=0.112).
Table 4. Frequency and percentage of clinical symptoms of dengue patients by occupation in Bangladesh (N=375).
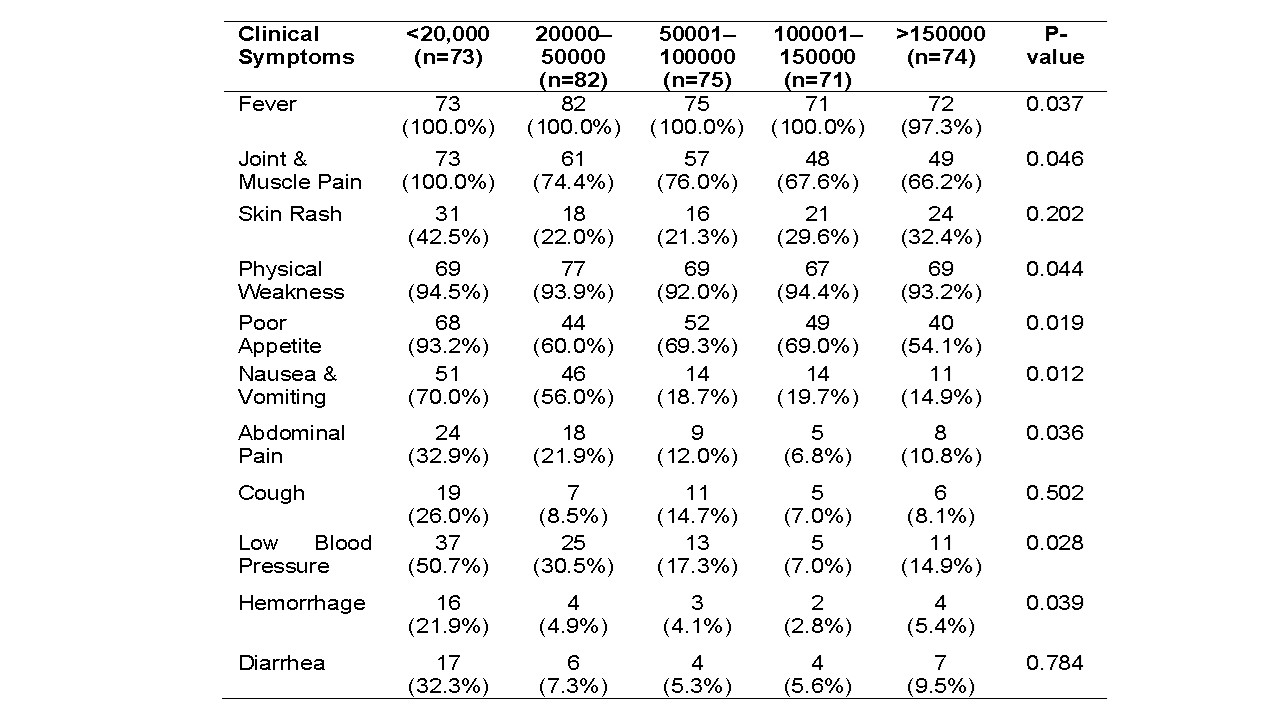
Analysis of clinical symptoms in Table 5 revealed significant associations between platelet count and symptom severity. The prevalence rate of any type of clinical feature was alarmingly higher for the <20,000/μL platelet count group compared to others. Along with fever, joint and muscle pain and physical weakness were most prevalent in the <20,000/μL group (100%) and least in the >150,000/μL group (66.2%, p=0.046). Skin rash peaked at 42.5% in the <20,000/μL group but was not significant (p=0.202). Poor appetite was most frequent in the <20,000/μL group (93.2%) and least in the >150,000/μL group (54.1%, p=0.019). A comparison between <20,000/μL and >150,000/μL, nausea and vomiting (70.0% vs. 14.9%, p=0.012), abdominal pain (32.9% vs. 10.8%, p=0.036), low blood pressure (50.7% vs. 14.9%, p=0.028), and hemorrhage (21.9% vs. 5.4%, p=0.039) were significantly more prevalent in lower platelet count groups. Diarrhea (p=0.784) and cough (p=0.502) showed no significant association. These findings indicate that severe thrombocytopenia (<20,000/μL) is strongly linked to warning signs and hemorrhagic manifestations, suggestive of severe dengue.
Table 5. Distribution of clinical symptoms of dengue patients by platelet count category.
As shown in Table 6, among the most common symptoms, joint pain (p=0.009), physical weakness (p=0.013), abdominal pain (11.1% vs. 82.3%), low blood pressure (15.2% vs. 52.9%), and hemorrhagic symptoms (5.0% vs. 61.7%) were significantly more common in patients experiencing a second dengue infection (p < 0.05). Other symptoms, such as nausea, vomiting, and cough, were also more frequent during secondary infections, though these differences were not statistically significant. These findings suggest an increased risk of severe physical complications during secondary dengue infections.
Table 6. Physical complications of dengue patients by number of infections.
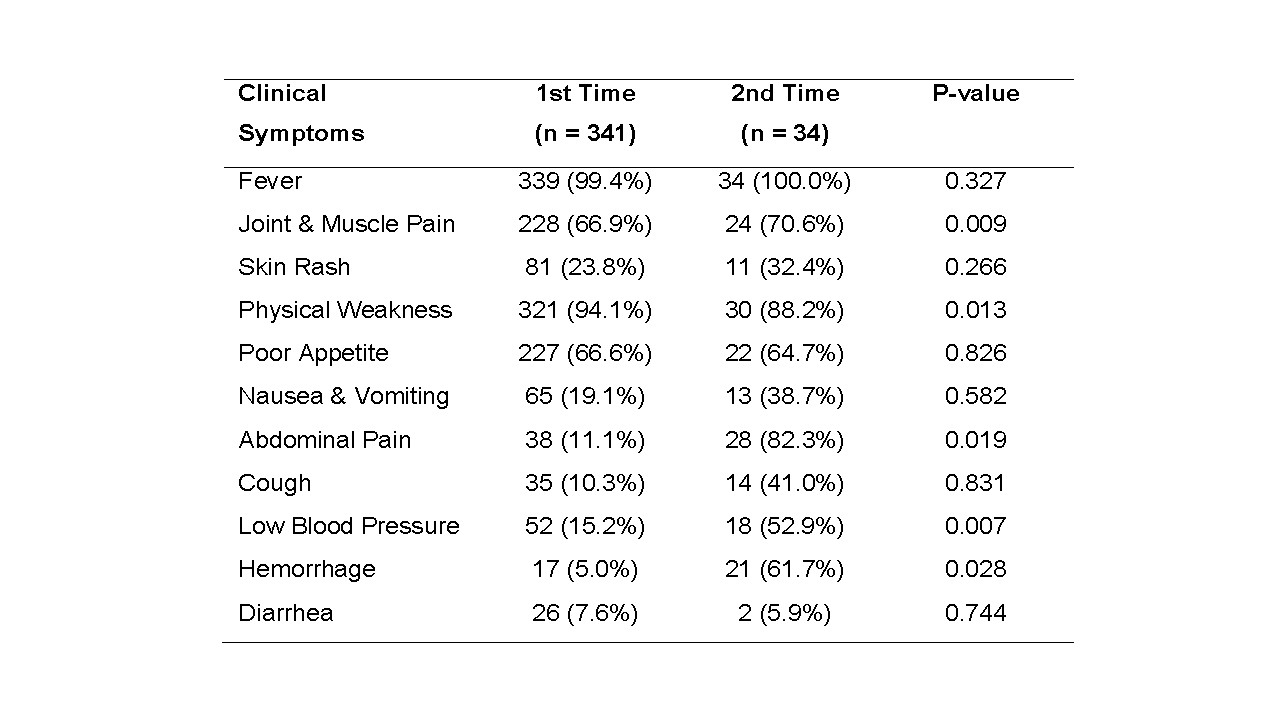
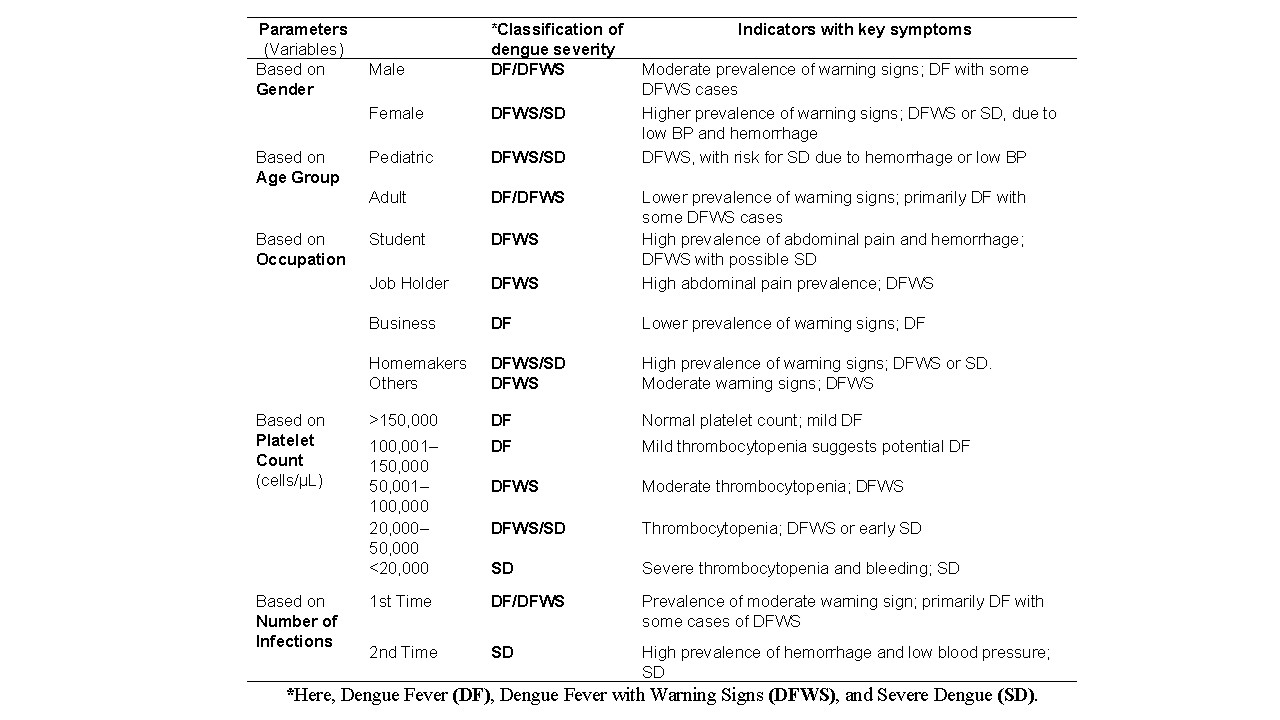
Table 7 presents the categorization of dengue severity based on clinical symptoms, as per the WHO 2009 guidelines [2], mediated by demographic and biochemical factors including age, gender, occupation, platelet count and number of infections of a patient. Here, females (n=139) exhibited a higher prevalence of warning signs (nausea/vomiting: 68.5%, low blood pressure: 49.2%, hemorrhage: 31.5%) compared to males (n=235; 53.2%, 31.7%, 19.4%, respectively), indicating DFWS or SD. Pediatric patients (n=97) showed higher warning signs (abdominal pain: 25.8%, nausea/vomiting: 25.8%) than adults (n=255; 6.3%, 16.5%), suggesting DFWS with potential SD. By occupation, homemakers (n=65) had the highest warning signs (nausea/vomiting: 50.8%, low blood pressure: 46.4%, hemorrhage: 27.2%), followed by students (n=97; abdominal pain: 43.8%, hemorrhage: 24.4%) and job holders (n=99; abdominal pain: 47.3%), indicating DFWS or SD, while the business group (n=29) showed milder DF symptoms (hemorrhage: 14.2%). Platelet counts <20,000/μL (n=73) were associated with severe symptoms (nausea/vomiting: 70.0%, low blood pressure: 50.7%, hemorrhage: 21.9%), aligning with SD, while counts >150,000/μL (n=74) indicated milder DF (hemorrhage: 5.4%). Second-time infections (n=34) had significantly higher warning signs (abdominal pain: 82.3%, low blood pressure: 52.9%, hemorrhage: 61.7%) than first-time infections (n=341; 11.1%, 15.2%, 5.0%), suggesting SD.
Table 7. Classification of dengue severity based on the clinical symptom by demographic and other biochemical factors.
The sociodemographic profile indicated a higher proportion of dengue fever cases among males than females, possibly due to greater occupational and outdoor exposure to mosquito vectors [16]. Our findings revealed that young and adolescent males were predominantly affected, followed by jobholders and homemakers (Table 1). Although female infection rates were lower, they exhibited more severe clinical complications than males. The distribution of dengue symptoms as indicators for severity presented in Figure 1, shows that patients experienced with diverse clinical manifestations of dengue. Nearly all patients experienced fever (99.0%–100.0%) and physical weakness (90.5%–98.9%), consistent with global findings, reflecting viral effects such as cytokine-mediated fatigue [17]. Fever, the most prevalent symptom, followed by physical weakness and abdominal pain, indicative of severe infection. Conversely, symptoms like diarrhea and cough were less common, suggesting moderate severity [17,18].
In this study, the influencing roles of some demographic factors (like gender, age, and profession) and biochemical factors such as platelet count, primary or secondary infection, and as a determinants of dengue symptoms and severity were evaluated systematically. Gender-based differences in symptomatology among male and female may reflect biological and immunological factors [19]. Females reported significantly higher rates of diarrhea, potentially linked to estrogen's (hormone) effects on gut permeability and mucosal immunity [19–21]. Higher incidences of nausea, vomiting, and hypotension among females may relate to hormonal modulation of serotonergic pathways, visceral sensitivity, and endothelial permeability [22, 23]. Increased hemorrhagic manifestations in females may result from estrogen’s influence on platelet function and coagulation [24]. Although females got stronger immune responses, these may also impair dengue symptoms and severity [25]. Sociocultural factors, such as healthcare-seeking behaviors, may further contribute to these observed differences with male.
Age was another significant determinant of severity (Table 3). Pediatric patients demonstrated a higher prevalence of warning signs and severe dengue (DFWS/SD), in line with previous studies attributing this to age-related immune response differences [26, 27]. Low blood pressure and hemorrhage were common across age groups but more noticeable in children, which may be due to increased vascular permeability [28]. Other symptoms like cough and diarrhea, which were not statistically significant, may indicate co-infections [29]. Occupation also prejudiced clinical outcomes of dengue parents. Homemakers reported a higher incidence of dengue compared to other groups, possibly due to delayed healthcare access and prolonged exposure to domestic mosquito habitats [30, 31]. Dehydration-related hypotension was more prevalent among homemakers, potentially due to lifestyle and hydration differences [32]. Other symptoms, including joint pain, skin rash, and hemorrhage, did not differ significantly across professions, suggesting viral and host factors are more influential than occupation [33].
Biochemical parameters, particularly platelet count, strongly correlated with dengue severity. Patients with severe thrombocytopenia (<20,000/μL) exhibited higher rates of warning signs such as nausea, abdominal pain, low blood pressure, and hemorrhage—indicator of SD, especially Dengue Shock Syndrome (DSS) [34, 35]. These findings align with WHO 2009 guidelines and support platelet counts <50,000/μL, particularly <20,000/μL, as predictors of severity [2, 36]. Non-significant symptoms like cough and diarrhea may reflect co-infections or non-specific presentations [37]. These results underscore the need for platelet count monitoring in dengue-endemic settings like Bangladesh, particularly during monsoon seasons [38]. Secondary infections were strongly associated with severe clinical consequences, including abdominal pain, hypotension, and hemorrhage, supporting the Antibody-Dependent Enhancement (ADE) mechanism [39, 40]. This immunopathological response, triggered by prior dengue exposure, likely contributes to increased vascular permeability and cytokine storms. Abdominal pain emerged as a key warning sign in secondary cases [41], emphasizing the need for close monitoring in previously infected patients.
Therefore, this study documented key demographic and biochemical predictors of dengue severity (Table 7). Females and pediatric patients were more likely to develop DFWS/SD, potentially due to hormonal and immunological factors [42]. Homemakers faced higher severity, possibly due to environmental exposure and healthcare access limitations. Severe thrombocytopenia and secondary infections were strongly associated with SD and DSS, consistent with global evidence [13, 43]. These findings highlight the importance of targeted surveillance and early intervention among high-risk groups in Bangladesh to mitigate severe outcomes during dengue outbreaks [27].
This patient-based study identifies critical demographic and biochemical predictors of dengue severity in an endemic region of Bangladesh. Female and pediatric patients, homemakers, individuals with severe thrombocytopenia, and those with secondary infections were at significantly higher risk for developing warning signs and severe dengue. The results emphasize the importance of incorporating gender, age, occupation, and platelet count monitoring into early diagnostic and management protocols. Personalized public health interventions targeting these high-risk groups, especially during peak transmission seasons, are crucial to reduce morbidity and mortality associated with dengue outbreaks.
We extend our heartfelt gratitude to all those who contributed to the successful completion of this research project. We are immensely grateful to all three-hospital authority, who allowed us to interview their patient`s, for the collection of data and report.
This research was conducted with self-funding. Therefore, any kind of financial support was not received for this study.
The authors declare no conflict of interest. All aspects of this research were conducted impartially and independently. No financial or personal relationships with other people or organizations have influenced this work.
This study did not involve any experiments on human participants or animals; therefore, formal written informed consent was not required. However, oral consent was obtained from all participants prior to data collection. Moreover, ethical approval was obtained from the Institutional Review Board of Primeasia University (PAU) (Ref: PAU/IEAC/22/12) prior to data collection, ensuring the privacy and confidentiality of participants were upheld throughout the study.